
OVERVIEW
This project aims to explore the connection between familial health management and emotional bonds, with the goal of addressing the lack of health awareness and management capabilities among middle-aged individuals and their adult children due to generational gaps, differences in health literacy, and lifestyle choices.
As parents transition from caregivers to care recipients, the ability and responsibility to manage health begin to shift to the next generation. How can we establish effective and easily acceptable family health connections to help alleviate the psychological stress of parents during this transition period? At the same time, how can we empower children who care for their parents to truly become new family caregivers, enhancing their own health management awareness and motivation as they aid their families?
We aspire to enhance the recognition of the unparalleled role the family unit plays as a participant in maintaining health and preventing disease, emphasizing the importance of mutual support and nurturing within the family throughout all stages of life.
DISCOVER
Early Context
- Record number of ambulances queue at A&E
- Ambulances taking 90 minutes to get to 999 calls
- ‘My dying husband could not get an ambulance’
- As the aging process intensifies and the susceptibility to chronic diseases increases, the NHS system, designed 75 years ago, faces new and increasing challenges to deliver care that meets the needs of current and future patients. People encounter difficulties in accessing high-quality and timely healthcare.
- At the same time, the UK government is under financial pressure. While maintaining the NHS budget, it has cut the budgets of local authorities. The services of local authorities cover expenditures such as public health, social care, transportation, housing, and environment, all of which are ‘social determinants of health’.
The Challenge
How can we cope with the current situation, and intervene through design to help alleviate the pressure on the NHS?
Early Strategy
- Strategy: Follow the design process of the double diamond model, guided by evidence-based design.
- Methodology/Tools: Case study, questionnaire, observation, in-depth interview, culture probe.
The first round of research – Community-centered attempts
- We believe that instead of ‘fixing’ the NHS, what is more essential is to fundamentally rethink how we approach health. Specifically, we should adopt a ‘proactive health’ approach that enables citizens to attain health, rather than depending solely on treatment.
Proactive health definition: Active health implies individuals having stronger self-repair and organizational abilities, greater physiological reserves, and higher levels of life satisfaction, resulting in positive physiological and psychological states. It stimulates the body’s self-organizing capabilities to eliminate diseases and promote health. It focuses on controlling health risk factors, deepening health concepts, enabling citizens to understand health, possesses basic health knowledge and skills, and thus achieve self-regulation and health management.
- People’s participation in community-centred health management services is low.
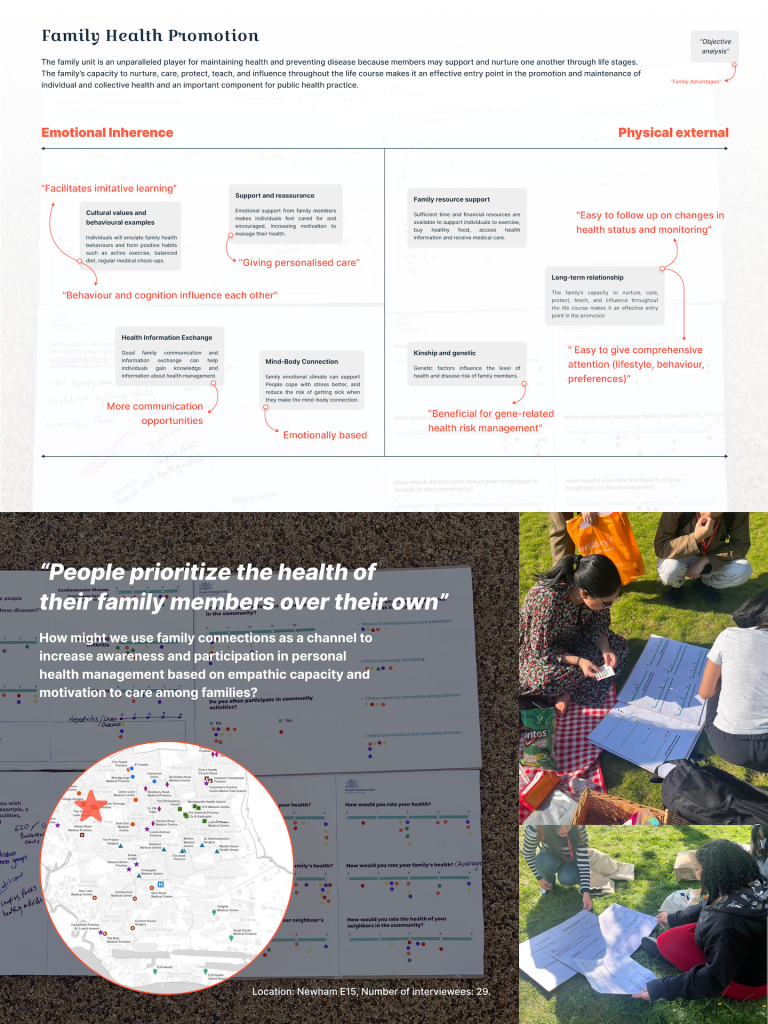
The second round of research – Priority family-centered
We have conducted an analysis of the key influencing factors and challenges that impact individuals’ proactive health management behaviours from perspectives such as personal behaviour, industry status, and social environment. We have also considered the value of the family setting in addressing these challenges and identified opportunities for intervention within the family context.
Family members can support and nurture each other at various stages of life, and the ability of families to nurture, care for, protect, educate, and influence makes them an effective entry point for promoting and maintaining individual and collective health. They are also an important component of public health practices.

DEFINE
Empathy with relatives is an important motivation for people to pay attention to health.
“People prioritize the health of their family members over their own, and the incentive to act on it is stronger.”
During our user interviews, we identified the critical opportunity point of ‘family caregivers’. How might we use family connections as a channel to increase awareness and participation in personal health management based on empathic capacity and motivation to care among families?
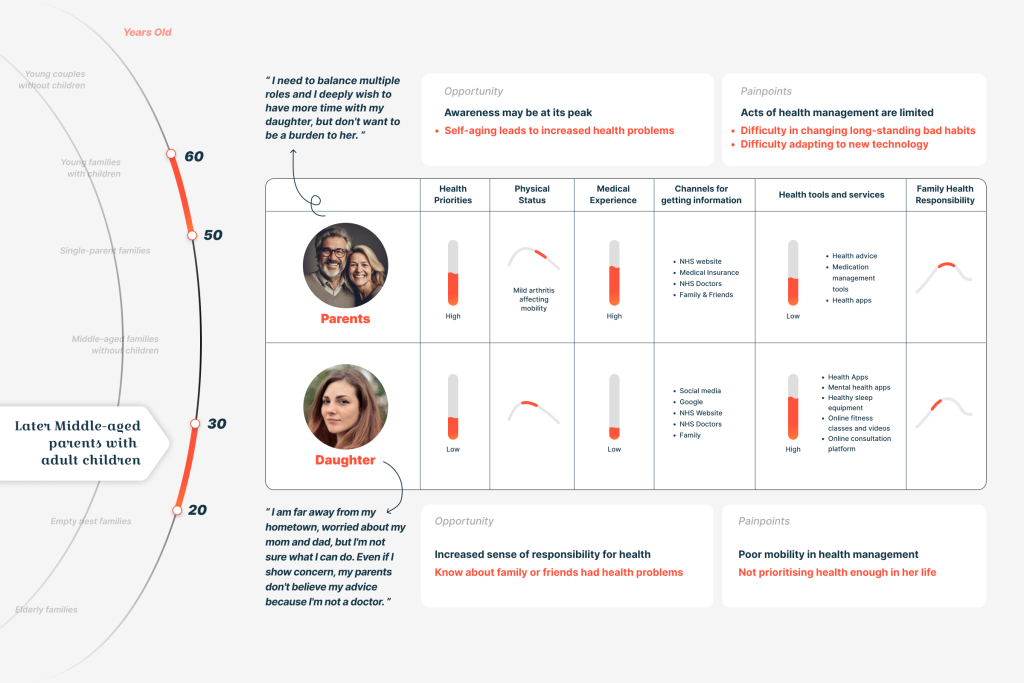
At different stages of life, each family member may potentially assume the role of a caregiver for health. However, the transitions between life stages can be key awakening periods for our care towards the health of our family members, leading to changes in our understanding and approach to health management. Therefore, we specifically focus on the intergenerational health relationships within families, particularly later middle-aged parents and their adult children. We analyze the pain points and opportunities in terms of health awareness and behaviours for both generations in the family, as well as the challenges faced in caring for each other’s health.
PROBLEM STATEMENT
In a family, middle-aged parents confront multiple role pressures and health risks associated with declining physical functions. They find it challenging to effect positive changes due to ingrained habits and psychological burdens. Young adult children voice concerns about their health due to work-related stress, but their limited time and experience impede their capacity to take proactive measures. The generational gap hampers effective health support between parents and children.
DEVELOP
How might we leverage the advantages of different family roles to establish a healthy emotional connection between middle-aged parents and young adult children, while satisfying their individual needs and enhancing the family’s overall health management awareness and capabilities?
VALUE
For middle-aged parents:
- Help parents promote disease prevention and early intervention, and, more importantly, gradually relieve the burden of multiple roles in the family and prepare for the transition to old age.
For adult children:
- Help adult children better understand their parents’ health issues and needs, fulfil the sense of family values, and truly become new caregivers in the family.
- It helps alleviate the pressure of transferring family responsibilities to the children stage and, in the process, subtly arouses attention and concern for their health.
For the family:
- Reduce estrangement and misunderstanding, and help two generations better understand each other’s needs, challenges, and perspectives.
- Form a closer family health network, create a family health atmosphere, and enhance the intimacy and emotional connection among family members.
For the community and public systems:
- Promote cooperation and resource integration between different organizations within the community and public systems. This collaboration can strengthen the practical implementation of self-care policies in the public system, alleviating the pressure on the NHS medical system due to doctor-patient tensions.
For the health management industry:
- Adopt an integrated medical and emotional care model, providing comprehensive health management services.
- Encourage the inclusion of families in the industry’s service model, offering tailored health management plans and support for families, including family psychological and medical services, family lifestyle interventions, and family medical collaborations.
- Attract more families to pay attention to and participate in health management, increasing the potential market and demand.
Each generation plays a crucial role in both societal and familial dynamics, and individual awareness and abilities are unstable, limited, and easily influenced by multiple factors. Our services leverage family relationships, the values of different members, and behavioural patterns to harness the power of the family unit and create a strong support system. This enables family members to develop a positive mindset and focus on their own health and the health of their loved ones.
Reference
- Triggle, N., ‘The NHS Crisis – Decades in the Making’, BBC News, 2023, https://www.bbc.co.uk/news/health-64190440 [accessed 25 June 2023].
- Rees, S., Pickles, C., and King, P., ‘Reimagining Health: A Framing Paper’, REFORM, 2023, https://reform.uk/publications/reimagining-health-a-framing-paper/ [accessed 25 June 2023].
- Stokes, Jonathan, Peter Bower, Bruce Guthrie, Stewart W. Mercer, Nigel Rice, Andrew M. Ryan, and Matt Sutton, ‘Cuts to Local Government Spending, Multimorbidity and Health-Related Quality of Life: A Longitudinal Ecological Study in England’, The Lancet Regional Health – Europe, 19 (2022), https://doi.org/10.1016/j.lanepe.2022.100436 [accessed 25 June 2023]
- Gao, Xiang et al., ‘Dilemma Analysis of Health Management Among Community Residents and Countermeasures Based on the Proactive Health Index’, Chinese Journal of General Practitioners, 22.01 (2023), 24-28 DOI:10.3760/cma.j.cn114798-20220810-00840.
- ‘Long-Term Conditions and Multi-Morbidity’, The King’s Fund, 2012, https://www.kingsfund.org.uk/projects/time-think-differently/trends-disease-and-disability-long-term-conditions-multi-morbidity [accessed 25 June 2023].
- Furman, D. et al., ‘Chronic Inflammation in the Etiology of Disease Across the Life Span’, Nature News, 2019, https://www.nature.com/articles/s41591-019-0675-0 [accessed 25 June 2023].
- ‘NHS Long Term Plan’, n.d., https://www.longtermplan.nhs.uk/online-version/overview-and-summary/ [accessed 26 June 2023]
- Infurna, F. J., Gerstorf, D., and Lachman, M. E., ‘Midlife in the 2020s: Opportunities and challenges’, American Psychologist, 75.4 (2020), 470-85. DOI: https://doi.org/10.1037/amp0000591. PMID: 32378943; PMCID: PMC7347230.
- Thomas, P.A., Liu, H. and Umberson, D., ‘Family relationships and well-being’, Innovation in aging (2017), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5954612/ [accessed 26 June 2023]
- Antti Tanskanen and Mirkka Danielsbacka, Intergenerational Family Relations: An Evolutionary Social Science Approach (London: Routledge, 1st edn, 2018)